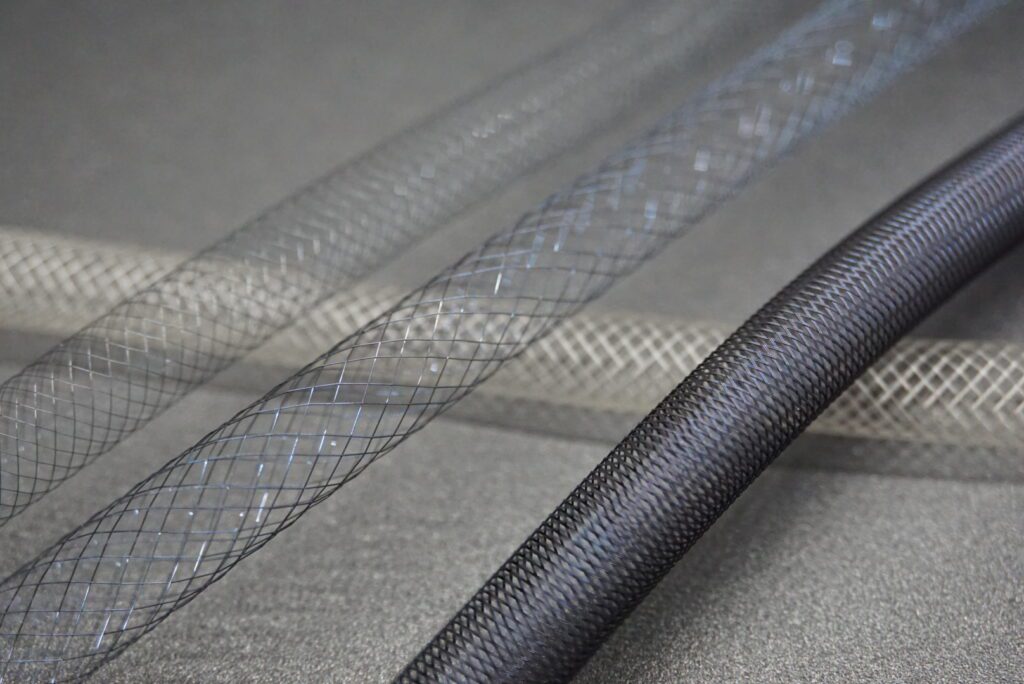
Braiding is a core technique in many interventional medical devices. Most people know braiding from its role in reinforcing catheter shafts, but it also plays a critical role in devices like thrombectomy tools, embolic filters, septal occluders, left atrial appendage (LAA) implants, and even some stents. The braid pattern and material choice have a big impact on how the device performs inside the body.
In this post we’ll explore the fundamentals of braiding, its application across a broader range of interventional and implantable devices (including thrombectomy devices, embolic filters, septal occluders, left atrial appendage (LAA) closure implants, stents, etc.), the most common metals and polymers used, and how braid geometry and material choices influence device performance.
Braiding 101: What It Is and Why It Matters
Braiding weaves multiple thin wires or fibers into a tubular mesh. The way the braid is built (e.g. density, angle, filament shape) controls:
- Torque transmission
- Stiffness and pushability
- Ability to bend without kinking
- Radial strength and expansion
- Overall flexibility and feel
A dense braid tends to provide support and control. A more open braid tends to allow flexibility and smoother navigation.
Where Braiding Is Used
Braiding shows up across a wide range of interventional devices:
| Device Type | What the Braid Helps With |
| Steerable/deflectable catheters and delivery systems | In systems where shaft deflection or articulation is needed, braiding may be used in proximal segments for torque and push and then transition to more flexible braid/coil blends or polymer only sections distally. |
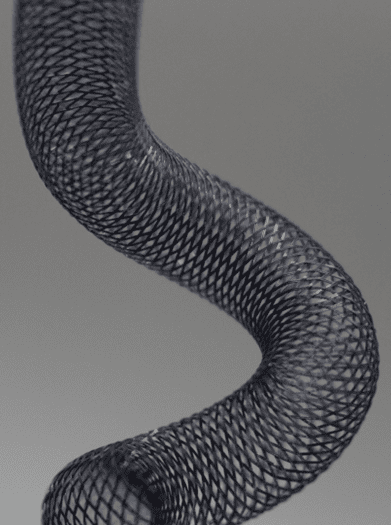
| Thrombectomy capture devices | In clot-retrieval systems (mechanical thrombectomy for stroke or pulmonary embolism), braided structures can form the capture basket, shell or scaffold that expands and collapses. The braid provides radial force to entrap thrombus, flexibility to navigate tortuous anatomy, and kink resistance during deployment and retrieval. |
| Embolic filters/deflectors | Embolic protection devices frequently use braided nitinol or polymer filaments to create fine mesh structures that allow flow but catch particulate. The braid geometry influences pore size, radial expansion, flexibility, and deployment profile. |
| Occluders & structural-heart implants | Devices like septal defect occluders or left atrial appendage (LAA) closure implants may use a braided frame (metal or polymer) that supports a fabric membrane. The braided frame must provide appropriate radial force, conformability, and minimal profile for delivery. |
| Stents, braided frames & covered stents | Braided metal or polymer frames serve as the structural skeleton in some stent designs. Compared to laser-cut stents, braided stents can offer more flexibility, better conformability, and incremental radial strength by tuning the braid pattern. |
| Other implants and scaffolds | Bioabsorbable scaffolds and polymer-fiber reinforcements for occlusion devices, vascular grafts or valve frames sometimes use braided fiber architectures for structural reinforcement. |
Common Metals and Polymers in Braiding
Selecting the correct filament material is essential for performance, biocompatibility, fatigue life, and manufacturability.
Metals
- Stainless Steel (304, 316L): Long-established for catheter shaft reinforcement.
- Nitinol: Superelasticity and shape-memory make nitinol the leading choice for implants, occluders, embolic filters, and braided stents.
- Platinum/Iridium, Tungsten, and Radiopaque alloys: Used for fluoroscopic visibility, sometimes blended with structural wires.
Polymers & Fiber Filaments
- Liquid Crystal Polymer (LCP): High strength and MRI compatibility.
- UHMWPE, PET, Kevlar, Carbon Fiber: Used where strength and thin wall profiles are needed.
- Bioabsorbable polymers (PLA, PLLA): Used for temporary scaffold designs.
- PEEK-based fibers: Used in hybrid structures or non-metal reinforcement.
Key Design Variables & Performance Impact
- Carrier count: More carriers → denser braid → higher torque & radial strength, less flexibility.
- Picks-per-inch (PPI): Higher PPI → more stiffness and hoop strength; lower PPI → greater flexibility.
- Braid angle: Low angle favors pushability; high angle favors radial force.
- Wire/fiber diameter and shape: Flat wires reduce wall thickness; round wires optimize smooth bending.
- Variable braid along shaft length: Enables balance of proximal strength with distal flexibility.
- Multi-layer braids: Used when distinct mechanical responses are needed in one structure.
Practical Guidance for Selecting Braid
- Define whether the device primarily needs support, flexibility, expansion, or shape retention.
- Choose metal vs polymer based on fatigue, radiopacity, MRI compatibility, and chronic implant vs temporary support.
- Collaborate early with the braiding and extrusion team to ensure manufacturability and smooth assembly transitions.
Example Device Scenarios
| Device Need | Example Braid Approach |
| Navigating small, tortuous brain vessels | Very fine stainless or LCP braid with lower density near the tip |
| Capture and remove clot in stroke | Nitinol braid that can expand and collapse repeatedly |
| Close an atrial septal defect | Braided nitinol frame that opens smoothly and holds shape |
| Temporary vascular support that dissolves | Bioabsorbable braided fibers with controlled resorption rate |
End-to-End Development
We design and manufacture braided reinforcement and braided device structures across the full development cycle:
- Material selection and braid pattern optimization
- Braid + extrusion + assembly integration
- Prototype builds and iterative refinement
- Scale-up into controlled manufacturing
Whether you are designing a new catheter shaft, developing an implantable filter or occluder, or exploring bioabsorbable scaffolds, our team can help you select and tune the right braid for your device’s performance goals.
Explore our online store to browse available braid samples. And if you’re ready to dive into braiding options for your next device, we’d be happy to connect.
